Could stem cells repair the damaged brain in Alzheimer’s?
Stem Cell Therapies: A Potential Cure for Alzheimer’s?
Understanding Alzheimer’s Disease

Alzheimer’s disease is a progressive and irreversible brain disorder characterized by symptoms such as disorientation regarding time and place, changes in mood, personality and behavior, memory loss, difficulty solving problems or planning, and difficulty writing or performing other routine tasks. This condition primarily affects people aged 70 years and above, with a higher prevalence in women. It is the main risk factor for dementia among the elderly.
Limitations of Conventional Treatments
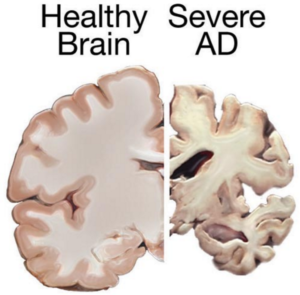
Currently, there is no known cure for Alzheimer’s. Conventional treatments, including both drug-based and non-drug strategies, may help with cognitive and behavioral symptoms but have little to no effect on the disease’s long-term progression. Medications available today cannot stop Alzheimer’s from progressing; they can only temporarily lessen symptoms like confusion and memory loss.
Exploring Stem Cell Therapies
Due to the limitations of conventional treatments, scientists are exploring the possibilities of stem cell therapies in Alzheimer’s treatments. Stem cells have the potential to develop new neurons, replace dead and damaged cells, and deliver neurotrophins to support neuron growth and survival.
Challenges in Developing Stem Cell Therapies
- Transplanting Neural Stem Cells:
- Theoretically, transplanting neural stem cells into the patient’s brain could generate healthy new neurons. However, it remains unclear whether the brain would integrate the transplanted cells effectively and if they could travel to the damaged areas.
- Producing the different types of neurons needed to replace the damaged cells and stimulating the renewal of lost connections between neural cells pose significant challenges.
- Delivering Neurotrophins:
- Neurotrophin proteins support neuron growth and survival, but Alzheimer’s patients produce insufficient amounts. Neural stem cells can produce these proteins, and studies in mice have shown some improvements in memory when treated with stem cells.
- Mesenchymal Stem Cells:
- Mesenchymal stem cells may exert anti-inflammatory effects and help ameliorate Alzheimer’s symptoms. However, there is currently no study proving their safety or effectiveness for this condition.
Research and Studies
Despite the high failure rate of clinical trials and studies on Alzheimer’s treatment, stem cells may still be valuable for studying the behavior of brain cells damaged by the condition. They can also be used for testing various therapeutic approaches and predicting which treatments might help Alzheimer’s patients.
- Induced Pluripotent Stem Cells (iPSC):
- Researchers from the Harvard Stem Cells Institute reprogrammed skin cells from Alzheimer’s patients to create iPSCs. These cells, grown in lab conditions, released the same proteins that form plaques in Alzheimer’s patients. This advancement allows scientists to study Alzheimer’s-affected cells and test new remedies.
- Neuronal Cell Conversion:
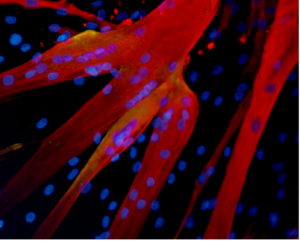
- Asian scientists turned human fibroblasts into neuronal cells using a chemical cocktail of small molecules. These findings provide an alternative strategy for modeling neurodegenerative disorders and may play a crucial role in identifying new stem cell-based treatments.
Conclusion
Stem cell therapies hold promise for developing new treatments for Alzheimer’s disease. While many challenges and uncertainties remain, ongoing research offers hope for understanding and potentially curing this debilitating condition.
References
- Published in Corporate News / Blog
New Stem Cell Research Shows Promising Results for Muscular Dystrophy
Understanding Muscular Dystrophy
Muscular dystrophy (MD) encompasses a group of genetic disorders that cause progressive muscle weakness and loss of muscle mass. These disorders, affecting primarily skeletal muscles, can also impact respiratory and swallowing muscles, leading to severe disability over time.
Types and Impact of Muscular Dystrophy
There are various types of muscular dystrophy, with Duchenne muscular dystrophy (DMD) being the most severe and common form, primarily affecting young boys. DMD is characterized by a genetic mutation that prevents the production of dystrophin, a crucial protein for muscle function. This deficiency leads to progressive muscle degeneration, loss of mobility, and, in many cases, premature death.
Current Treatments and Limitations
Currently, there is no cure for DMD. Treatment focuses on managing symptoms and slowing disease progression through therapies like physiotherapy and steroids. However, these treatments have limitations and often come with significant side effects.
Potential of Stem Cell Therapies for Muscular Dystrophy
Regeneration with Stem Cells
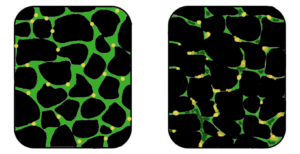
Stem cell research offers promising avenues for treating muscular dystrophy by targeting muscle regeneration. Studies have shown that stem cells isolated from muscle tissue, bone marrow, and blood vessels can potentially regenerate dystrophin-deficient muscle fibers in animal models.
Experimental Success with Stem Cells
Recent studies have demonstrated encouraging results in animal models of DMD. Researchers have successfully restored mobility in dogs and improved muscle function in mice by transplanting stem cells. These studies suggest that stem cells could potentially replace damaged muscle tissue and restore muscle function.
Combining Stem Cell and Gene Therapies
Emerging research also explores combining stem cell therapies with genetic correction techniques. This approach aims to correct the genetic defect responsible for DMD and stimulate muscle regeneration simultaneously, showing promising outcomes in preclinical studies.
Future Directions and Research
While the application of stem cell therapies for DMD in humans is still in its early stages, ongoing research holds significant promise. Future studies will focus on optimizing stem cell treatments, enhancing their safety and efficacy, and ultimately translating these findings into viable therapies for patients with muscular dystrophy.
Conclusion
Stem cell research represents a beacon of hope for advancing treatment options for muscular dystrophy, particularly DMD. As research progresses and clinical trials continue, the potential of stem cells to regenerate muscle tissue and improve quality of life for patients with muscular dystrophy becomes increasingly promising.
References:
- http://www.mayoclinic.org/diseases-conditions/muscular-dystrophy/basics/definition/con-20021240
- http://www.eurostemcell.org/factsheet/muscular-dystrophy-how-could-stem-cells-help
- https://www.mda.org/disease/duchenne-muscular-dystrophy/research
- http://quest.mda.org/article/scientists-bullish-stem-cells-muscle-repair
- http://hsci.harvard.edu/stem-cells-used-treat-muscular-dystrophy-mice
- https://med.stanford.edu/news/all-news/2014/12/stem-cells-faulty-in-duchenne-muscular-dystrophy.html
- Published in Corporate News / Blog
Global Stem Cells Group to Hold Intensive, Two-day Training Course on Stem Cell Harvesting, Isolation and Re-integration Sept. 27 and 28 Following International Symposium
Global Stem Cells Group announced plans to hold a two-day, hands-on intensive stem cell training course at the Servet Clinic following the First International Symposium on Stem Cells and Regenerative Medicine in Santiago Chile, Sept. 26, 27 and 28, 2014.
Global Stem Cells Group, its subsidiary Stem Cell Training, Inc. and Bioheart, Inc. have announced plans to conduct a two-day, hands-on intensive stem cell training course at the Servet CordónVida Clinic Sept. 27 and 28 in Santiago, Chile. The “Adipose Derived Harvesting, Isolation and Re-integration Training Course,” will follow the Global Stem Cells Group First International Symposium on Stem Cells and Regenerative Medicine at the Santiago InterContinental Hotel Sept. 26, 2014.
Global Stem Cells Group and the Servet CordónVida Stem Cell Bank Clinic of Chile are co-organizing the symposium, designed to initiate a dialogue between researchers and practitioners and share the expertise of some of the world’s leading experts on stem cell research and therapies.
Servet CordónVida is a private umbilical cord blood bank that harvests and stores the hematopoietic-rich blood stem cells found in all newborns’ umbilical cords after birth. The hematopoietic tissue is responsible for the renewal of all components of the blood (hematopoiesis) and has the ability to regenerate bone marrow and restore depressed immune systems.
Umbilical (UCB) stem cells offer a wealth of therapeutic potential because they are up to 10 times more concentrated than bone marrow stem cells. In addition, UCB cells have a generous proliferative capacity with therapeutic potential that is very similar to embryonic stem cells, without the ethical debate associated with embryonic stem cell research and use.
UCB cells are the purest adult stem cells available, coming from newborns who have not been exposed to disease or external damage. Many parents today are utilizing cord banks like Servet CordónVida to store their newborn’s UCB cells safely for future medicinal use if the need arises.
Global Stem Cells Group and Servet CordónVida represent a growing global community of committed stem cell researchers, practitioners and investors whose enthusiasm is a direct result of the hundreds of diseases and injuries that stem cell therapies are curing every day. Global Stem Cell Group’s First International Symposium on Stem Cell Research and Regenerative Medicine will host experts from the U.S., Mexico, Greece, Hong Kong and other regions around the globe who will speak on the future of regenerative medicine and share experiences in their field of specialty. The Global Stem Cells Group is hoping the symposium will open lines of communication and cooperation, explore new and exciting techniques in stem cell therapies, and create an environment of education and learning.
- Published in Press Releases




