Stem cell treatment could offer one-end-solution to Diabetes
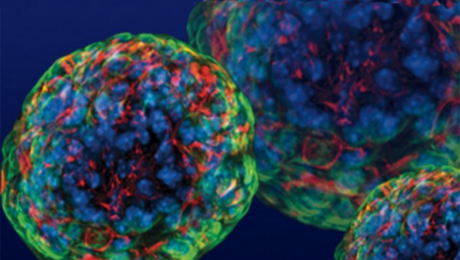
Insulin-producing cells grown in the lab could provide a possible cure for the age-old disease, diabetes.
Understanding Type 1 Diabetes
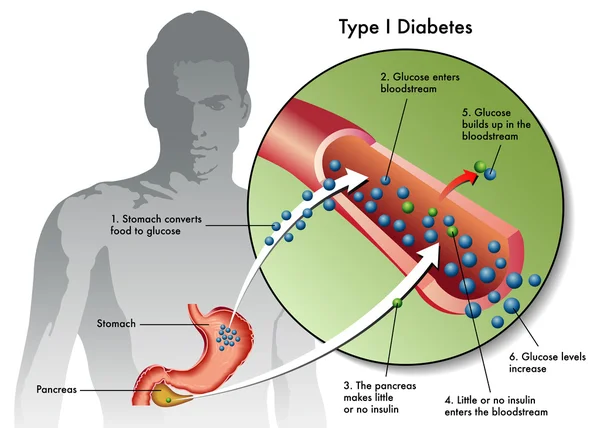
Type 1 diabetes is an autoimmune disease that destroys insulin-producing pancreatic beta cells, leading to dangerously high blood glucose levels. Patients often require insulin administration and other medications to manage blood sugar levels. For those who struggle with blood sugar control, beta-cell transplants are an option, but they require immunosuppressive drugs.
Breakthroughs in Stem Cell Research
A research group at Harvard University reported using insulin-producing cells derived from human embryonic stem cells (ESCs) and induced pluripotent stem cells to lower blood glucose levels in mice. Laboratories worldwide are making rapid progress in human stem cell technology to develop cells functionally equivalent to beta cells and other pancreatic cell types. Novel biomaterials are being developed to encapsulate these cells, protecting them from the immune system without the need for immunosuppressants.
Major Investments in Diabetes Treatment
Pharmaceutical companies and venture capital firms have invested over $100 million in leading biotechnology companies to bring stem cell treatments into clinical use. Prominent companies include:
- Semma Therapeutics
- Sigilon Therapeutics
- ViaCyte
Transforming Human Stem Cells into Insulin-Producing Cells
Researchers at UC San Francisco have successfully transformed human stem cells into mature insulin-producing cells, a significant breakthrough in developing a cure for Type 1 Diabetes (T1D). These cells mimic the function of pancreatic beta cells and offer hope for creating transplantable cells for patients with diabetes.
What is T1 Diabetes?
Type 1 diabetes is characterized by the destruction of insulin-producing beta cells in the pancreas, typically starting in childhood. Without insulin, blood glucose levels can spike, causing severe organ damage and potentially leading to death. The condition can be managed with insulin shots, but serious health complications often persist, such as kidney failure, heart disease, and stroke.
Making Insulin-Producing Cells from Stem Cells
Diabetes can be treated through a pancreas transplant or donor cell transplantation, but both methods rely on deceased donors. Scientists have struggled to produce mature beta cells responsive to blood glucose and capable of secreting insulin correctly. However, recent breakthroughs at UCSF have achieved this transformation in mice, marking a critical step toward human application.
Protecting Stem Cell Therapies from the Immune System
Delivering stem cell therapies requires protection from immune attacks while maintaining cell functionality. Companies are exploring two main strategies:
- Microencapsulation: Immobilizing cells individually or in small clusters within biocompatible gel blobs.
- Macroencapsulation: Placing larger numbers of cells into a larger, implantable device.
Companies Leading the Way
- ViaCyte: Partnered with Johnson & Johnson, using microencapsulation in clinical trials.
- Semma: Developing both macro- and microencapsulation methods, readying for clinical trials.
- Sigilon: Utilizing gel-based spheres for encapsulation, in collaboration with Eli Lilly.
Conclusion
Stem cell treatment holds the potential to revolutionize diabetes care, offering a one-end solution to managing and potentially curing the disease. With significant investments and ongoing research, the future of diabetes treatment looks promising. Researchers and companies are making strides in developing effective and safe stem cell therapies, bringing hope to millions worldwide.
- Published in Corporate News / Blog
Insulin-producing Stem Cells Grown in the Lab Mark a New Era in Stem Cell Therapies for Diabetes
Introduction to Insulin-Producing Pancreatic Beta Cells
A new discovery by researchers on how to activate lab-grown beta cells to mature into functioning cells that produce and release insulin in response to glucose takes a significant step toward a cell therapy treatment for diabetes. Difficulties in manipulating beta cells derived from human stem cells to mature beyond the precursor stage into fully functioning insulin releasers have been an ongoing challenge for researchers.
Breakthrough by Salk Institute Researchers
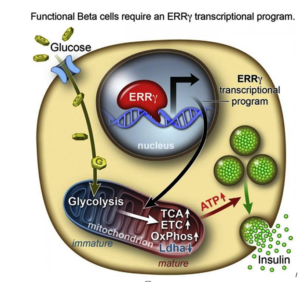
However, researchers from the Salk Institute for Biological Studies and a team of researchers have achieved this goal with lab-grown beta cells by activating a protein called estrogen-related receptor γ (ERRγ). Their study findings were recently published in the journal Cell Metabolism.
The Role of Human Pluripotent Stem Cells (hPSCs)
Ronald Evans, senior author of the study titled, “ERRγ Is Required for the Metabolic Maturation of Therapeutically Functional Glucose-Responsive β Cells,” explains the self-renewing capacity of human pluripotent stem cells (hPSCs) and their ability to differentiate into most cell types—from neurons to skin cells, to muscle cells, and insulin-producing pancreatic beta cells—has inspired many research teams to find ways to make glucose-responsive beta cells in the lab. Evans and his research team discovered the answer to the insulin-releasing cell conundrum, and summed it up thusly: “In a dish, with this one switch, it’s possible to produce a functional human beta cell that’s responding almost as well as the natural thing.”
Challenges in Lab-Grown Pancreatic Beta Cells
Evans, a molecular biologist at the Salk Institute, says that to create the different types of cells in the lab, researchers coax the pluripotent stem cells (hPSCs) down the various branching paths that fetal cells normally travel in order to differentiate into the various cell types. However, he explains there are many developmental points in this process, and in the case of lab-grown pancreatic beta cells, research kept getting stuck at an early stage.
Role of ERRγ in Adult Beta Cells
In order to determine what might trigger the next step in getting the cells to mature, the researchers compared transcriptomes of adult and fetal beta cells. The transcriptome contains, among other things, the full catalog of molecules that switch genes on and off in the genome, which led them to discover that the nuclear receptor protein ERRγ was more abundant in adult beta cells. The team was already familiar with the protein’s role in muscle cells and had studied its ability to enhance endurance running. Evans says that in muscles, the protein promotes greater growth of mitochondria—the power generators inside cells that accelerate the burning of sugars and fats to make energy.
Surprising Findings on Beta Cells
“It was a little bit of a surprise to see that beta cells produce a high level of this regulator,” Evans says. “But beta cells have to release massive amounts of insulin quickly to control sugar levels. It’s a very energy-intensive process.” The research team then decided to run some tests to look more closely at what role ERRγ might play in insulin-producing beta cells.
A New Era in Creating Functional, Insulin-Producing Beta Cells

After they genetically engineered a deficiency of ERRγ in mice, the researchers found the animals’ beta cells did not produce insulin in response to spikes in blood sugar. Next, they tried to get beta cells made from hPSCs to produce more ERRγ, and it worked! The cells in culture began to respond to glucose and release insulin. Finally, the team transplanted the lab-grown insulin-producing beta cells into diabetic mice and found that from day one, the cells produced insulin in response to glucose spikes in the animals’ blood.
Future Implications and Research
Evans and the research team were justifiably excited by the results. It appears that just switching on the ERRγ protein is sufficient to get the lab-grown beta cells to mature and produce insulin in response to glucose – both in cultures and in live animals. Speculating on the implications of their findings, Evans suggests that when a fetus is developing, because it gets a steady supply of glucose from the mother, it does not need to produce insulin to regulate its blood sugar, so the switch is inactive. But, when the baby is born and takes its first breath and takes in oxygen, this activates the switch. Previous lab attempts to produce beta cells got stuck at the fetal stage. The Salk Institute researchers discovered how to take it to the adult stage, using the same protein that is switched on in nature.
Conclusion
“I believe this work transitions us to a new era in creating functional beta cells at will,” Evans says. He and his research team now plan to examine how the switch might work in more complex models of diabetes treatments. The Salk Institute study precedes another study reported by Medical News Today in which researchers generated mini-stomachs that produce insulin when transplanted into mice.
- Published in Corporate News / Blog

![Secondary-Diabetes[1]](https://www.stemcellsgroup.com/wp-content/uploads/2020/02/Secondary-Diabetes1-460x260_c.png)